Congestive Heart Failure Transcript
Congestive Heart Failure
This is Dr. Cal Shipley with a review of congestive heart failure.
Cardiopulmonary Physiology
Let’s start by reviewing cardiac and pulmonary physiology. The heart lies between the lungs in the middle of the chest cavity, also known as the thorax. Let’s zoom in to take a closer look at the heart. There are four chambers within the heart. On the left side, the left atrium and the left ventricle, and on the right side, the right atrium and right ventricle.
Systole and Diastole
The movement of blood through the heart is divided into two distinct phases, systole and diastole, which together are known as the cardiac cycle.
During systole, both the right and left ventricles contract. With contraction, the right ventricle pumps deoxygenated blood into the lungs, and the left ventricle pumps freshly oxygenated blood into the aorta.
During diastole, both ventricles relax and refill with blood. The right ventricle fills with deoxygenated blood flowing from the right atrium, which in turn receives blood from the venous system, while the left ventricle fills with freshly oxygenated blood flowing from the lungs via the left atrium.
Pulmonary Blood Circulation
Now let’s take a closer look at the circulation of blood through the lungs. The right ventricle accepts deoxygenated blood from the venous system via the right atrium, and pumps the blood through the pulmonary artery into the lungs, where it is freshly oxygenated. The freshly oxygenated blood is returned to the heart through the pulmonary veins into the left atrium and then into the left ventricle. The left ventricle then pumps the oxygen-rich blood into the aorta, and hence, to all organs and tissues of the body.
Congestive Heart Failure
Now that we’ve done a review of basic cardiopulmonary physiology, it’ll be easier to understand the concept of congestive heart failure.
The primary component in most cases of congestive heart failure is impairment of left ventricular function. The impairment may occur during systole, so-called systolic congestive heart failure, or during diastole, diastolic congestive heart failure. Overall, about 60% of individuals with CHF have systolic dysfunction.
Systolic Congestive Heart Failure
Let’s start with a review of systolic congestive heart failure. The essence of systolic congestive heart failure is the failure of adequate emptying of the left ventricle during systole. Let’s see what we mean by that.
Left Ventricular Ejection Fraction
Returning to a cross-sectional view of the heart, let’s take a closer look at the function of the left ventricle. The effectiveness of left ventricular contraction is described by a term known as ejection fraction also known as EF. At rest between contractions, the left ventricle fills with blood coming from the lungs. With contraction, only a portion of the total blood in the left ventricle is pumped into the aorta. The ratio of the blood volume pumped into the order to the volume of blood present in the left ventricle after filling is the ejection fraction.
This ratio is generally expressed as a percentage, a normal ejection fraction for an adult human being is between 50% and 70%. In conditions where the contraction of the left ventricle is impaired, the portion of blood pumped into the aorta by the left ventricle will decrease, and this decrease, in turn, will be reflected by a reduced value for the ejection fraction.
Causes of Systolic Congestive Heart Failure
While there is a long list of conditions which can impair left ventricular function and result in congestive heart failure, the four most common are coronary artery disease (and its consequences), myocardial ischemia and heart attack (also known as myocardial infarction), disease of the cardiac muscle (also known as cardiomyopathy), valvular disease, and high blood pressure (also known as hypertension).
Consequences of reduced Ejection Fraction
As can be seen in this comparison, maximum contraction of the impaired left ventricle is clearly reduced compared to normal, and along with a reduced pumping action goes a reduced ejection fraction. The consequence of an abnormally reduced ejection fraction in an impaired left ventricle is that the volume of blood ejected by the ventricle with each contraction is less than the volume of blood flowing to the ventricle from the lungs. This results in a backup of blood flow and therefore an increase in blood pressure within the blood vessels of the lungs.
Pulmonary Edema
Blood vessels are relatively porous structures and become more so as the pressure of the fluid within them increases.
Fluid in the form of serum begins to leak from the blood vessels in the lung. The presence of abnormal amounts of fluid outside the vasculature of the lung is known as pulmonary edema and is a hallmark of congestive heart failure. Oxygen absorption is impaired and results in shortness of breath, a common presenting symptom of congestive heart failure. Red blood cells often accompany the serum that makes up the fluid of pulmonary edema, and affected individuals often cough up a characteristic frothy pink sputum.
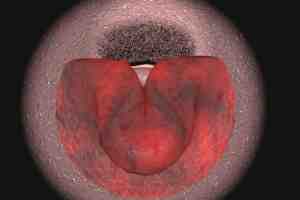
Auscultation of the Lungs in Pulmonary Edema
Listening with a stethoscope, the breath sounds of an individual in acute pulmonary edema have a characteristic underwater quality. Following is a comparison of normal breath sounds with those heard in acute pulmonary edema.
[breath sounds]
Diastolic Congestive Heart Failure
Diastolic congestive heart failure represents the opposite side of the coin in that it is caused by inadequate filling of the left ventricle during diastole.
Here’s a comparison on the left of a normally functioning left ventricle, and on the right, a left ventricle with diastolic dysfunction. Stopping the animation at the point of maximum ventricular relaxation during diastole, it can be seen that the blood volume in the abnormal ventricle is significantly less than the blood volume in the normal ventricle. The decreased filling volume of the abnormal ventricle relates to an inability to relax or stiffness of the cardiac muscle and has the same underlying causes as those mentioned for systolic dysfunction. The decreased filling volume of the left ventricle and diastolic dysfunction has the same effect on blood circulation through the lungs as systolic dysfunction. Because the left ventricle can accept less blood per cycle, blood flow through the lungs is backed up, resulting in increased pulmonary blood pressure, leakage of fluid and pulmonary edema.
Ejection Fraction in Diastolic Congestive Heart Failure
One interesting aspect of diastolic congestive heart failure is the fact that ejection fractions are almost always normal. This is so often the case that by definition, congestive heart failure in the presence of an ejection fraction of greater than 50% is considered to be due to diastolic dysfunction until proven otherwise.
The fact that ejection fraction is normal in diastolic congestive heart failure may seem counterintuitive until one considers two factors: First, while the capability of the left ventricle to relax and expand its volume in diastolic CHF is significantly impaired, contractility is often near normal, so the ventricles’ ability to eject blood is often preserved. Second, while the ejection fraction maybe 50% or more, it’s 50% of a much smaller filling volume than in a normal left ventricle, and so the actual volume of blood injected into the aorta is significantly smaller as depicted here.
Cal Shipley, M.D. copyright 2020