LVAD Left Ventricular Assist Device CVS181
LVAD Left Ventricular Assist Device Transcript
LVAD Left Ventricular Assist Device
This is Dr. Cal Shipley with a review of the left ventricular assist device. In order to better understand how the left ventricular assist device works, let’s take a look at some normal cardiac physiology.
Cardiac Physiology
In a normal heart, the primary blood pumping chambers are the left and right ventricles. The left ventricle pumps oxygenated blood through the aorta to all bodily organs and tissues. Oxygen-poor blood returns to the heart via the venous system and is pumped through the lungs by the right ventricle.
Left Ventricular Failure
Failure of the left ventricle occurs when muscular contraction of the ventricular wall is severely impaired, which may occur, for example, as a result of acute myocardial infarction.
In this example, normal right ventricular contraction and function has been preserved. In left ventricular failure, oxygenated blood output from the left ventricle is critically reduced. As a result, the volume of blood returning to the heart is also reduced.
Left Ventricular Assist Device (LVAD)
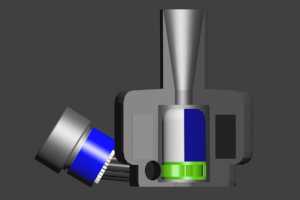
Let’s take a look now at the left ventricular assist device, also known as an LVAD. Here is an example of a typical state-of- the-art LVAD unit employing Mag/Lev design.
LVAD Structure
Most of the components of an LVAD pump consist of metal such as titanium, which is lightweight, durable, and has a very low degree of chemical interaction with bodily tissues and fluids. On top of the pump is the inflow cannula, a hollow metal tube through which the pump receives blood from the left ventricle.
The pump housing contains a rotor which is attached to an impeller. The impeller drives blood into an outflow channel. The housing contains electromagnets, while the rotor contains permanent magnets. An electrical current is applied to the electromagnets via an external power controller. The magnetic field of the electromagnets interacts with the permanent magnets in the rotor and causes it, and its attached impeller, to rotate.
Magnetic Levitation
The Mag/Lev (or magnetic levitation) feature of the pump is a piece of engineering genius. Magnets in the pump housing interact with the rotor magnets causing it to float within the pump housing chamber. This design eliminates the need for supportive bearings which would physically attach the rotor to the pump housing.
The end result of the magnetically levitated rotor is a less turbulent flow of blood through the pump compared to a conventional bearing supported design. Less turbulent flow translates to less chance of dangerous clot formation.
Texturing and Endothelial Stimulation
In addition, all the inner surfaces of the pump over which blood flows are textured with titanium microspheres. The microspheres stimulate production of endothelial tissue, which coats the surfaces preventing blood contact with artificial materials, further reducing the chance of clot formation.
Blood Flow Through The LVAD
Blood flows from the left ventricle into the pump through the inflow cannula, and is then driven by the impeller into the outflow channel.
Maglev style LVADs are continuous flow pumps and are capable of circulating 8 to 10 liters of blood per minute.
LVAD Placement
To place the LVAD, the chest wall and ribs must be surgically opened in order to access the left ventricle. Once the heart has been adequately exposed, the patient is placed on cardiopulmonary bypass. The cardiopulmonary bypass system takes the place of the heart and lungs throughout the procedure oxygenating blood and circulating it through the vascular system.
A medication known as a cardioplegic is administered intravenously in order to stop the heart from beating during the implantation of the LVAD.
Device Implantation
Once the patient has been safely placed on cardiopulmonary bypass, and the heartbeat has been stopped with cardioplegics, the implantation procedure for the LVAD may proceed.
The surgeon uses a specialized coring tool to create a tunnel through the wall of the left ventricle at its apex. The inflow cannula of the pump is then inserted through the tunnel into the left ventricle.
The collar of the LVAD pump is affixed to the left ventricle with a series of sutures. A grafting tube typically made of polyester is attached to the LVAD pump and sutured to the ascending aorta.
LVAD Function
Let’s switch to a cross-sectional view of the heart to better understand how the LVAD works in the left ventricular failure.
The LVAD pumps blood from the impaired left ventricle to the aorta. As a result, oxygen-rich blood flow to organs and tissues (including the heart) itself is much increased. The increase in arterial blood flow is accompanied by a comparable return of venous blood to the right ventricle.
A normally functioning right ventricle can cope with the increased return of venous blood. The other side of this coin is that patients who have left ventricular failure and are candidates for an LVAD device must have normal or near-normal function of their right ventricles.
LVAD with Left and Right Ventricular Failure
To illustrate this point, let’s take the example of a patient affected by cardiomyopathy where there is both left and right ventricular failure present. In this scenario, the LVAD device still results in a dramatic improvement of oxygen-rich blood flow from the left ventricle into the arterial system. The impaired right ventricle, however, cannot cope with the LVAD- mediated increase in venous blood return. Blood backs up in the right ventricle resulting in progressive ventricular enlargement and eventual collapse of cardiac function.
Cal Shipley, M.D. copyright 2020