Hemifacial Microsomia ENT071
Hemifacial Microsomia Transcript
Hemifacial Microsomia
This is Dr. Cal Shipley with a review of hemifacial microsomia. A quick word on nomenclature, hemifacial microsomia is also known by a variety of other names. One of the most commonly used alternatives is craniofacial microsomia.
Anatomy of the Embryo
In order to better understand the underlying causes and pathogenesis of hemifacial microsomia, let’s take a look at some embryological anatomy, starting with the branchial arches.
The Branchial Arches
Here is a human embryo at approximately four weeks of growth. The branchial arches, also known as pharyngeal arches, develop to form structures of the face, skull, and ear. The first branchial arch develops into the maxilla and mandible, as shown here, as well as the malleus and incus, two of the three bones comprising the middle ear, and a number of other facial bones, muscles, and ligaments. (You can see a complete list of structures derived from the first arch by following the link on this page).
The second branchial arch develops into the stapes, the third of the three bones in the middle ear, as well as the muscles of facial expression. (Please go to the link on this page to view a complete list of the second branchial arch derivatives).
The Neural Tube
Running the length of the four-week-old embryo is the neural tube. This will eventually develop into the central nervous system, including the brain and spinal cord.
Embryo Vascular System
At just four weeks of development, the heart is already active and circulating blood throughout the embryo with a pulse rate of about 120 beats per minute. Each of the branchial arches has an artery dedicated to its blood supply.
Development of Craniofacial Structures
Now let’s turn to the process by which the branchial arches develop into the craniofacial structures previously mentioned.
The Neural Crest
Stretching across the top (roof) of the neural tube is a layer of cells known as the neural crest. The neural crest is present on both the left and right sides of the neural tube. Neural crest cells are a form of stem cell from which specialized cells may develop to generate bone, cartilage, muscles, connective tissue, nerves, and pigment.
The portion of the neural crest located at the cranial end of the neural tube contains cells which will ultimately form the cranial facial tissues in the first and second branchial arches. Neural crest cells achieve this through the processes of migration and specialization.
Neural Crest Cells
Let’s take a closer look at these amazing cells. Like most of the cells in the human body, neural crest cells have a nucleus which contains DNA. DNA is the blueprint for the production of all organs and tissues in the human body. The structure of DNA was first discovered by Watson and Crick in the 1950s. DNA consists of a double helix, within which are connected pairs of nucleic acids (also known as bases).
There are four nucleic acid bases: adenine, guanine, cytosine, and thymine. Chains of these nucleic acid bases arranged in varying orders provide the code from which all animal and plant life on the earth is derived.
For the most part, DNA enables this incredible task by encoding for hundreds of thousands of different proteins, each protein with a special job to perform. The production of specialized proteins is critical to the function of human neural crest cells.
Protein Production
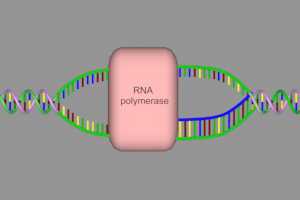
Let’s take a closer look at how the production of proteins occurs. The first step on the road to protein production is for an enzyme called RNA polymerase to unwind the DNA strands. The bases are now exposed and the RNA polymerase, in a process known as transcription, duplicates a sequence of bases which are encoded for a particular protein. The duplicated base sequence created by RNA polymerase is known as messenger RNA. The sequence of bases that encodes for a particular protein is known as a gene.
Once produced, the messenger RNA binds to a ribosome, the protein assembling unit of a cell. The ribosome facilitates the assembly of proteins via another kind of RNA known as transfer RNA. Each transfer RNA molecule carries a particular amino acid. Amino acids are the building blocks of protein.
In the ribosome, three base combinations on the messenger RNA strand attract transfer RNA molecules with a particular amino acid attached. The transfer RNA binds to the messenger RNA and releases its amino acid. This process, known as translation, repeats and the ribosome assembles the amino acids into a complete protein.
For purposes of illustration today, I’m showing a protein consisting of only five amino acids, but in fact, the smallest proteins in the human body contain at least 100 amino acids, and the largest comprise a chain of over 30,000.
Role of Proteins
Many different proteins, all with a particular task, are produced in a neural crest cell. These proteins are involved in a complex pattern of interaction, which signals the cell to migrate to the branchial arches and controls cell specialization once there.
Proteins also enable cell-to-cell signaling to coordinate migration and specialization.
Neural Crest Cell Migration
Under the control of proteins, the neural crest cells migrate to the first and second branchial arches. This process occurs on both the left and right side. Once in the brachial arches, the neural crest cells specialize and divide to form facial jaw and ear structures as the embryo develops.
Hemifacial Microsomia
Now that we know a little bit more about the key stages in the development of the facial structures, let’s look at hemifacial microsomia.
Definition of Hemifacial Microsomia
By definition, hemifacial microsomia involves underdevelopment of facial structures on one side of the face relative to the other side. The ear and lower jaw are most commonly affected, but abnormalities of the tongue, mouth, and eye may also be involved. In some cases, both sides of the face may be affected, often to varying degrees. Abnormalities may vary from mild to severe.
Incidence of Hemifacial Microsomia
The incidence of hemifacial microsomia is approximately one in 5,000 live births, and in terms of congenital craniofacial abnormalities, it occurs with a frequency which is second only to clefts such as cleft lip or cleft palate.
Causes of Hemifacial Microsomia
The root cause of hemifacial microsomia is inadequate embryonic activity of neural crest stem cells in the first and second branchial arches. Much research has been devoted to uncovering specific causes for the impairment in stem cell potential in this disorder. To date, the only cause for which there is solid scientific evidence is an inheritable genetic form of the disease. In this inheritable form, one or both parents of the affected child carries the gene for HFM.
Inheritable Hemifacial Microsomia
As mentioned previously, a gene is simply a collection of nucleic acid bases on the DNA strand. The specific gene sequence for HFM in human DNA has not yet been discovered, but it is likely that it interferes with the production of normal signaling proteins in the neural crest cell. The HFM gene, as well as a sequence of base codes encoding for proteins, is copied and converted to messenger RNA by RNA polymerase.
Translation Blocking
One theory is that the HFM gene acts by blocking translation of signaling protein genes at the ribosome. Production of proteins critical to migration and specialization of neural crest cells is impaired and normal development of craniofacial features from the first and second branchial arches cannot proceed.
Forms of Inheritable Hemifacial Microsomia
The genetically inheritable form of HFM occurs in an autosomal dominant variety in which only one parent needs to carry the gene in order to pass it on to their child. The chance of inheritance with this form is 50%.
There is also an autosomal recessive variety in which both parents must carry the gene in order to pass it on to a child. The chance of inheritance with this variety is 25%.
Environmental Toxins and Genetic Damage
Another proposed but as yet, unproven cause of HFM involves genetic damage caused by environmental toxins. The toxins are passed from mother to fetus and then interfere with neural crest cell protein production, either through damage to protein genes on the DNA strand, or inhibition of RNA polymerase activity during transcription.
Branchial Arch Vascular Insufficiency
Vascular insufficiency to the branchial arches has also been proposed as a possible cause of HFM. In this scenario, the dedicated arteries to the first and second branchial arches are severely underdeveloped thus depriving the arches of the oxygen and nutrients required for normal facial structure formation and growth.
Trauma In Utero
Finally, physical trauma experienced during pregnancy has been proposed as a possible cause of HFM.
Physical Manifestations of Hemifacial Microsomia
To complete this presentation, let’s take a look at how a typical case of hemifacial microsomia manifests itself. By a typical case, I mean a child affected by abnormalities of the lower jaw and the ear, the two manifestations of HFM which most commonly occur. additional abnormalities of facial structures may be present in any given case.
The Mandible in Hemifacial Microsomia
The lower jaw is formed by the mandible. The mandible articulates with the temporal bone of the skull to form the temporomandibular joint.
Temperomandibular Joint
The TM joint is unique in that it is bilateral. There is both a left and right temporomandibular joint and these two joints must function together in order to allow normal opening and closing of the jaw.
Malformation of one temporomandibular joint, as may occur in HFM, may have a significant impact on the overall function of the joint especially during chewing.
Mandibular Condyle and Ramus
At the tip of the condylar process of the mandible is the condyle. The condyle articulates with the mandibular fossa of the temporal bone to create the temporomandibular joint. The ramus connects the condylar process with the lower half of the mandible.
In microsomia, the condylar process and ramus are underdeveloped and smaller than normal. This results in angling of the jaw with deviation of the chin toward the affected side. This gives the affected child the characteristic appearance of hemifacial microsomia.
The Ear in Hemifacial Microsomia
As mentioned, the ear is commonly affected in HFM. The size and shape of the external ear may be abnormal. The middle ear may also be affected with under-development of one or more of the ossicles. In this example, the incus is underdeveloped resulting in a loss of contact with the stapes. This interrupts the transmission of sound vibrations from the tympanic membrane (eardrum) to the inner ear and results in hearing impairment on the affected side.
If you’re interested in more information on HFM, please explore the links on this web page.
Cal Shipley, M.D. copyright 2020