Aortoiliac Graft Procedure for Abdominal Aortic Aneurysm VAS123
Aortoiliac Graft for Abdominal Aortic Aneurysm Transcript
Aortoiliac Graft for Abdominal Aortic Aneurysm
This is Dr. Cal Shipley with a review of aortoiliac bypass graft to treat abdominal aortic aneurysm.
The placement of an aortoiliac bypass graft is a complex surgical procedure. While many such cases move smoothly from start to finish, others may present the surgeon with one or more challenges along the way. Fortunately, today’s vascular surgeons are highly trained and skilled in both anticipating, and resolving, such issues. In this presentation, I’ll be showing you a few examples of these surgical “bumps in the road and how surgeons deal with them.
Aortoiliac Graft Procedure
Transperitoneal and Retroperitoneal Organ Exposure
The procedure typically begins with a midline incision in the abdomen. The peritoneal membrane, which enfolds the abdominal contents, is opened, and the intestines are displaced to expose the posterior peritoneal wall. The posterior peritoneal wall is opened to expose the aorta and the iliac arteries. This surgical approach to the aorta and iliac arteries is known as the transperitoneal approach and involves cutting through the peritoneal membrane, both in its anterior and posterior walls.
Many surgeons are now using a retroperitoneal approach to expose structures such as the aorta and spine. A retroperitoneal approach avoids incision of the peritoneal membrane. You can find out much more about the retroperitoneal approach by reviewing my video in the orthopedics library.
Abdominal Aortic Aneurysm
This enlarged, very irregular area of the abdominal aorta represents an aneurysm. Looking at the aneurysm in cross-section reveals a smaller pouch-like aneurysm located just above the main lesion. Blood flowing by this pouch has become trapped and formed a clot. If left intact, the clot from this pouch could travel distally, potentially blocking blood flow to the lower limbs, so it too will need to be bypassed by the graft.
Proximity to Renal Artery
In this particular example, the top of the aneurysmal pouch is located just below the junction of the right renal artery and the aorta. The right renal artery is the primary source of blood flow to the right kidney. This is an important decision point for the vascular surgeon as he must accurately assess whether or not he can attach the bypass graft to the aorta and successfully bypass the pouch without interfering with the right renal artery. Here is a left lateral view of the aneurysm, the pouch containing the clot, and the take-off of the right renal artery.
In this example, the surgeon makes the judgment that the graft can be safely attached to the aorta without interfering with the right renal artery.
Iliac Artery Aneurysms
It is not uncommon for large abdominal aortic aneurysms to be accompanied by aneurysms of one or both of the iliac arteries, as shown here. Large aneurysms of the iliac arteries are prone to rupture and/or dissection, and must also be bypassed by the placement of the graft. These aneurysms may extend to the origins of the internal iliac arteries.
Internal Iliac Arteries
The internal iliac arteries are a major source of blood flow to the pelvic organs and tissues, and so they must be preserved in the process of attaching a bypass graft. In view of this, the surgeon will have to decide how best to proceed with the attachment of the iliac artery limbs of the bypass graft.
Exposure of the Aorta, Renal Arteries and Illiac Arteries
To begin, the tissues around the left and right renal artery are dissected to more fully expose them and their anatomical relationship to the aorta and the aneurysm. A vessel loop is placed around the right renal artery at the point of its origin from the aorta to pinpoint its location, and prevent back-bleeding during the procedure.
In similar fashion, the iliac arteries are then exposed down to the origin of the internal iliac arteries. Tissue is then dissected away from the aorta to expose it at the neck of the aneurysm.
Aortic Friability and Bleeding
Large aneurysms are typically associated with advanced atherosclerotic disease of the aorta. The condition of the aortic wall may be described as friable – subject to tearing with the manipulation required to place a bypass graft. Tearing of the wall may manifest itself as a pinhole bleeder as shown here. When bleeding occurs, suction is used to keep the operative field exposed.
Sutures are used to close the pinhole. A suture is threaded through a felt pledget to provide a more secure closure of the pinhole.
In the presence of a friable aortic wall, even the tension associated with the tying of sutures may cause new tears. These new tears will result in further bleeding. To gain control of the situation, it may be necessary for the vascular surgeon to apply a clamp across the aorta above the point of bleeding.
Opening the Aneurysm
With the bleeding controlled, the pinhole bleeder is set aside for the moment and the surgeon places clamps across both the external and internal iliac arteries. A T-type incision is used to open the aneurysm.
Repair of Pinhole Bleeder and Aortic Tears
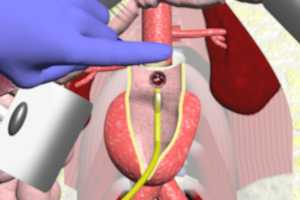
The surgeon now turns his attention to the pinhole and suture-related tears. The previously placed aortic cross-clamp must be removed in order to fully expose and allow for a secure repair of the tears. The surgeon applies finger pressure across the aorta just below the clamp, so that when the clamp is removed blood will not flood the operative field. An occlusion balloon attached to a catheter is inserted into the aorta and then inflated to stop blood flow and allow repair. The pinhole and suture tears may now be fully inspected from the inside of the aorta, allowing for a more secure repair using multiple pledgets. The synthetic aortoiliac graft is now ready for placement.
Placement of the Aortoiliac Graft: Aortic Segment
The graft is composed of a synthetic material such as Dacron, and has an aortic segment and two iliac limbs. The occlusion balloon catheter has been threaded through the graft so that the balloon may remain in place until the aortic segment of the graft has been attached. The graft is placed end to end with the aorta and a felt collar is wrapped around the junction to strengthen the connection. Sutures are placed circumferentially through the felt collar to sew the aorta and graft together. Clamps are applied across the iliac limbs of the graft and the occlusion balloon is deflated to test the aorta graft connection.
If there is no blood leakage noted at the aorta graft junction, the connection is deemed to be sound. The occlusion balloon and catheter are removed and the surgeon turns his attention to attachment of the iliac limbs.
Placement of the Aortoiliac Graft: Iliac Limbs
The iliac limb clamps previously applied are kept in place for this part of the procedure. The right internal and external iliac arteries are cut and then syndactylized, (joined together) so that blood flowing through the iliac limb of the graft will supply flow to both arteries with a single connection. The right limb of the graft is then attached to the syndactylized arteries. Good pulses are noted in both arteries and there is no leakage of blood at the junction.
The left external and internal iliac arteries are now cut. However, on this side, the arteries cannot be syndactylized.
This can occur for a variety of reasons, including friability of the arteries (which could result in tearing of the artery walls when they are pulled together), the presence of scar tissue in the area from a previous pelvic injury or infection, limiting mobility of the arteries, or an aneurysm which extends into either or both of the arteries requiring a more distal cut, which leaves the distance between the arteries too great to allow for syndactylization. In this circumstance, the left limb of the graft is attached directly to the external iliac artery.
No Pulses after Graft Attachment
In this example, after the attachment of the limb graft, there is no palpable femoral artery pulse in the left groin. Palpation of the external iliac artery by the surgeon raises suspicions of a blockage, either by a clot or atherosclerotic plaque, located just beyond the graft-artery connection. A jump graft is attached to the graft limb and to the external iliac artery beyond the point of the suspected blockage. A good femoral artery pulse is now palpable, indicating that the use of the jump graft has been successful.
An additional jump craft is used to attach the graft limb to the internal iliac artery. A good pulse is noted in the artery.
“Jacketing” of the Graft
Successful attachment of the graft is complete. The remains of the aneurysm are closed over the graft like a jacket to prevent adhesion of abdominal tissues. The aortoiliac bypass graft procedure is complete.
Cal Shipley, M.D. copyright 2020