Pericardiocentesis CVS065
Pericardiocentesis Transcript
Pericardiocentesis and Cardiac Tamponade
Cardiac Anatomy
This is Dr. Cal Shipley with a review of pericardiocentesis. Let’s start by taking a look at some relevant cardiac anatomy.
In the front (anterior) aspect of the rib cage, the sternum acts as an anchor to which all ribs, and rib cartilage, attach. Projecting from the bottom of the sternum is the xiphoid process also known as the xiphisternum. Lying just behind the xiphoid process is the left lobe of the liver. Removing the rib cage reveals the lungs. Between the lungs is the pericardial sac which contains the heart.
Let’s move in for a closer look:
The pericardial sac completely encloses the heart. The purpose of the pericardial sac is to protect the heart. It has attachments to the diaphragm and to the back (posterior) aspect of the sternum and so physically anchors the heart within the thorax, thereby reducing the potentially adverse effects of upper body movement on cardiac function.
The pericardial sac also isolates the heart from other organs within the thorax, particularly the lungs, and via the pericardial fluid, which we will look at next, provides a friction-free environment for cardiac activity.
Finally, the pericardial sac acts as a physical barrier to infection which might otherwise spread to the heart as a result of infection of other organs within the thorax.
The Pericardial Sac
Now, let’s take a look at the pericardial sac in a cross-sectional view.
The fibrous pericardium is the outermost layer and consists of dense connective tissue, and attaches the pericardium to the sternum and diaphragm, as mentioned previously.
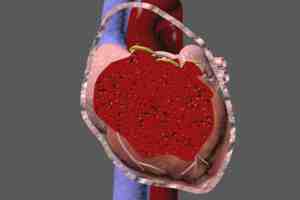
The innermost layer is known as the serous pericardium and is divided into two layers.: the parietal layer and the visceral layer. Between these two layers lies a potential space known as the pericardial space. Within the pericardial space resides the pericardial fluid. On cross-section, the thickness of the pericardial fluid is only about two millimeters. Under normal circumstances, the pericardial fluid volume is typically 30 to 50 cc, or 1 to 1 1/3 ounces.
This thin layer of fluid surrounds the heart and acts as a shock absorber, further reducing the impact of upper body movements on cardiac function. The pericardium fluid also provides a low friction environment for the contractions and expansions of the cardiac chambers.
Now let’s take a look at the pericardial sac and its various anatomical relationships from the left lateral point of view with the patient lying down. We see the pericardial sac with the diaphragm beneath it. Under the diaphragm is the left lobe of the liver. As can be seen, the xiphoid process lies just anterior to, (in front of) the diaphragm. Switching to a cross-sectional view of the pericardial sac reveals the heart within.
Pericardiocentesis Indications
Let’s take a look now at why we perform pericardiocentesis: to remove pericardial efffusions and prevent cardiac tamponade.
Returning to a view of the pericardial sack in cross-section reveals a normal pericardial fluid depth of about two millimeters, which again corresponds to about 1 to 1 1/3 ounces of pericardial fluid.
Pericardial Effusion
A pericardial effusion refers to an abnormal accumulation of fluid within the pericardial space.
Depending on the underlying cause, the effusion may consist of pericardial fluid, blood, purulent material, commonly known as pus, or a combination of any of the three.
Pericardial Effusion Causes
There are many possible underlying causes for a pericardial effusion. A few of the most common causes are malignancy, especially that of the breast or lung; infection, viral or bacterial; secondary to heart attack; trauma, including injury during medical procedures; and idiopathic (unknown). You can learn much more about the causes of pericardial effusion in my cardiac tamponade article. I’ve added a link to it on this web page.
This example shows a symmetrical distribution of the pericardial effusion around the heart. Irrespective of where it is measured, the pericardial fluid has about the same depth.
However, the pericardial effusion is very often asymmetrically distributed, as in this example, where the majority of the fluid is contained in the inferior (lower) aspect of the pericardial sac. The distribution of the effusion may be an important determining factor in choosing which pericardiocentesis approach to use.
Returning now to our symmetrically distributed effusion, in this example, the pericardial effusion has a depth of about 20 millimeters, or 10 times the normal thickness. This depth correlates to a volume of about 500 to 1000 cc of pericardial fluid. This represents about 20 times the normal volume of fluid within the pericardial space.
A key factor in determining how much a pericardial effusion will affect the pumping action of the cardiac chambers is how rapidly the expansion of fluid volume occurs.
Chronic (Slow Onset) Pericardial Effusions
If the increase in pericardial fluid volume occurs slowly over a period of weeks to months, the pericardial sac is capable of expanding along with the fluid minimizing the effect on cardiac function. Under these circumstances, pericardial fluid volumes of up to 2,000 cc or about 50 times normal may be tolerated.
Acute (Rapid Onset) Pericardial Effusions
If, however, the effusion accumulates rapidly over a period of hours or a few days, the pericardial sac is unable to stretch enough to compensate. Increasing fluid pressure within the pericardial sac begins to inhibit the pumping action of the cardiac chambers.
Cardiac output begins to drop and the heart may initially be able to compensate by increasing pulse rate. As the pericardial effusion volume increases, the pressure on the cardiac chambers results in a critical reduction in cardiac output. Unless pericardiocentesis is performed on an emergency basis, cardiac arrest and death will soon follow. This is acute cardiac tamponade.
Typically in acute cardiac tamponade, the free walls of both the right ventricle and right atrium are collapsed because the right atrium and right ventricle have more compliant walls and are under lower pressure than the left atrium and left ventricle.
Pericardiocentesis Technique Considerations
Now that we have some understanding of the relevant anatomy and the concept of pericardial effusion and cardiac tamponade. Let’s take a look at pericardiocentesis.
The first step in pericardiocentesis involves using a needle to enter the pericardial space and the pleural effusion that lies within.
Pericardiocentesis Approaches
The three most commonly used approaches are, subxiphoid, as depicted here, where the needle is inserted just laterally to the xiphoid process of the sternum.
Parasternal, where the needle is inserted perpendicular to the patient’s body just lateral to the left border of the sternum, usually above the fifth or sixth rib.
The apical approach, where the needle is inserted five to six centimeters lateral to the sternal border, usually in either the fifth sixth or seventh intercostal space.
Choice of Approach
How does one choose which of these three approaches to use during emergent pericardiocentesis? Prior to the era of real-time ultrasound guidance, pericardiocentesis was performed blindly using pal patient and percussion of the chest wall in an attempt to determine where the pericardial effusion was deepest and hence which approach to use. This technique may still be used to determine the best approach in situations where real-time ultrasound guidance is unavailable.
Pericardiocentesis and Ultrasound
The use of ultrasound in pericardiocentesis can contribute in two important ways. Using ultrasound prior to needle insertion, the deepest part of the pericardial effusion can be more accurately determined. With this information in hand, the operator may choose the needle insertion approach, which will tap into the deepest area of the effusion. Additionally, once the needle insertion approach has been chosen, real-time ultrasound may be used to guide the needle into the effusion. This can reduce the chance of inadvertent injury to the cardiac chambers, coronary arteries or lungs.
In summary, the use of ultrasound in pericardiocentesis provides for a safer and more efficient procedure. In the United States, when available, using ultrasound in conjunction with pericardiocentesis has become the standard of care.
Pericardiocentesis Procedure
To look at the nuts and bolts of the pericardiocentesis procedure itself, I’m going to use, as an example, the subxiphoid approach. Please note that with the exception of the insertion point and the aiming of the needle, the technique is the same regardless of the approach used.
Let’s start with a quick recap of the relevant anatomy. The xiphoid process projects from the bottom of the sternum. Enclosing the heart, the pericardial sac rests on top of the diaphragm, and positioned just below the diaphragm is the liver. For this example, I’m going to use an effusion which is symmetrically distributed and is 20 millimeters in depth. This corresponds to an infusion volume of about 500 to 1000 cc of fluid. In order to reduce the risk of needle puncture or laceration of cardiac chambers or coronary arteries, the targeted area of the effusion should be at least 10 millimeters in depth.
With the subxiphoid approach, in the anterior-posterior orientation, the pericardial needle is aimed toward the left shoulder. In a lateral orientation, the needle is aimed at a 45-degree angle to the plane of the body. These aiming guidelines are used to start the insertion even when real-time ultrasound needle guidance is available. Though in the case of ultrasound-guided insertion, changes in the needle trajectory may be made on-the-fly.
With these guidelines in mind, the needle is then inserted through the gap that exists between the xiphoid process and the rib cage. Viewed from the lateral aspect, the 45-degree insertion angle avoids needle puncture of the diaphragm or liver.
In some cases, whether it’s anatomic variation or a highly domed diaphragm, as shown here, it is considered acceptable technique to puncture the diaphragm and/or the liver if it is determined that that is the best approach to the effusion.
As the needle is slowly advanced, gentle traction is applied to the plunger of the syringe. As the needle passes through the parietal layer of the pericardial sac and enters the effusion, fluid flows into the syringe. The syringe is detached from the needle.
A guidewire is inserted through the needle and into the pericardial effusion. The needle is then removed. A soft, flexible, pigtail catheter is advanced over the guidewire and into the pericardial space. The guidewire is now removed. The pigtail catheter is anchored to the external chest wall with sutures. Typically, a large barrel syringe is then attached to the pigtail catheter and the syringe used to actively remove pericardial effusion fluid until signs and symptoms of cardiopulmonary compromise has been relieved.
The pericardial effusion is resolved and cardiovascular collapse from acute cardiac tamponade is prevented.
Cal Shipley, M.D., copyright 2020